Over the past 10 + years there has been a massive increase in discussions around concussions. The topic seems to be everywhere—in professional sports such as football, hockey, soccer, legal battles between players and their leagues. And, amateur sports have also been in the headlines with one pro- found case resulting in the Ontario legislature passing a law referred to as “Rowan’s Law” — named for Rowan Stringer, a high school rugby player who died as a result of her multiple concussions (second impact syndrome). This law mandates that all school boards in Ontario have appropriate concussion prevention, recognition and management strategies in place. Despite all of the attention to concussions in the media there still seems to be a lot of confusion, misinformation and in many cases, poor management of concussions. Hopefully this article will help answer more questions than it creates.
There is a specific and technical definition of what we now consider a concussion, one that we will not bore you with: the scientific definition. The understanding of how a concussion occurs and the physiological changes within the brain which occurs as a result of trauma have changed. It was previously believed that as a result of a trauma such as a slip and fall, a punch or hitting the head into the boards in hockey, that the brain is slammed into the skull, back and forth causing a “Coup” or “Coup Contrecoup” mechanism. Such a violent insult would most likely result in focal brain injury bleeding or structural dam- age which is not observed or evident with concussions. The most recent, accepted understanding of a concussion also known as Mild Traumatic Brain Injury (MTBI) in briefest terms, is as a result of a traumatic event, the brain tissues are slightly stretched which causes a large number of neurons to fire simultaneously. This brings on mass firing of neurons resulting in the depletion of the brains energy sources at an incredible rate. This reaction in the brain causes the initial presentation of symptoms such as headache, nausea, vomiting, dizziness, confusion, sensitivity to light, balance problems and more, affecting every person differently or in varying degrees.
In addition to changing knowledge regarding the mechanics behind a concussion, previous beliefs regarding diagnosis and prevention have been disproven. Other common myths or misconceptions are that you have to strike your head, you must lose consciousness to have sustained a concussion, and that helmets and mouth guards help prevent concussions. The evidence is that you do not have to hit your head to suffer a concussion. Rapid acceleration/deceleration can be sufficient to cause a concussion. The majority of our patients who have sustained concussions have not lost consciousness and unfortunately there is no conclu- sive research evidence that helmets or mouth guard use reduces the risk of concussions.
Who is getting concussions?
Most people assume concussions primarily occur because of sports, particularly contact sports. While it is true that many who sustain a concussion are involved in sports, an increasing proportion of the patients we see at the clinic present with concussion symptoms related to slips and falls, work injuries and motor vehicle “whiplash” mechanism events. Any incident which introduces significant acceleration/deceleration forces in the head and neck can potentially create an injury and may cause a concussion.
A data collection organization which tracks ER (Emergency Room)vis- its and related diagnoses in Ontario reported that in 2010 there were a total of 13, 493 concussions diagnosed.
About 15% were related to motor vehicle accidents, 38% from falls, and 37% were from being struck by someone or against something. Data obtained in the USA between 2006-2011 shows 3.8 million concussions a year, with an estimated cost of $5.6 billion in healthcare costs. A review of numbers from WSIB (Workplace Safety and Insurance Board of Ontario) indicates in 2015 there were a total of 229,000 claims, 7-8% of which were classified as cranial/concussion injuries. This would mean greater than 16,000 work related concussions were diagnosed in 2015. This does not count many concussion injuries which are undiagnosed or misdiagnosed. A review of the existing data suggests that over 50% of all concussions are never reported or diagnosed.
 As it relates to sports the highest concussion rates are associated with Rugby (male and female) Hockey (male and female), Football (male), Lacrosse and Soccer (male and female). Concussions are also very com- mon and seem to be increasing in Alpine Skiing and Snowboarding; 11.8% of injuries sustained by competitive skiers/snowboarders are in- juries to the head/face of which 81.6% are concussions. Additionally, skiing and snowboarding combined account for 18% of all sports and recreational related injury hospitalizations in winter with 10-20% of in- juries to the head and neck.
As it relates to sports the highest concussion rates are associated with Rugby (male and female) Hockey (male and female), Football (male), Lacrosse and Soccer (male and female). Concussions are also very com- mon and seem to be increasing in Alpine Skiing and Snowboarding; 11.8% of injuries sustained by competitive skiers/snowboarders are in- juries to the head/face of which 81.6% are concussions. Additionally, skiing and snowboarding combined account for 18% of all sports and recreational related injury hospitalizations in winter with 10-20% of in- juries to the head and neck.
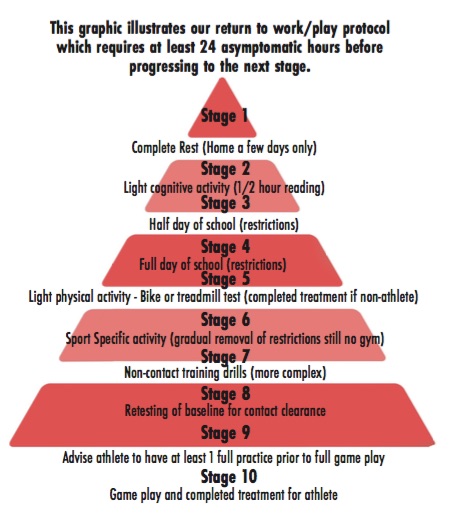
Evolving concussion management, responding to the research.Recommendations to patients who have been diagnosed with a concussion have traditionally been inconsistent and not well based in research. Recommendations for a return to normal activities of daily living including work, leisure and sports have traditionally been vague— “when you feel better”. Research has now provided us with much more structured treatment/management and return to play/activity recommendations.
For sport: the importance of a comprehensive baseline testing…
It has been recommended that concussion diagnosis involve detecting injury without grading severity (mild, moderate, or severe) and that de- cisions regarding return to play become more individualized. Having pre-season baseline results to pick up on slight alterations in cognitive and physical signs following a potential concussive injury is crucial to ac- curately identifying a concussion.
Administering a multimodal instrument (one which measures variable aspects of cognitive and physical function), as soon as reasonably pos- sible following a potential injury and comparing it to the baseline pre-in- jury results is a crucial step in the recognition and rehabilitation of a concussion.
It is important to understand what an athlete was like prior to a sus- pected concussion, in order to recognize if post-injury presentation is dif- ferent. There is increasing emphasis being placed on the objectivity of concussion assessment and the potential use of pre-participation baseline scores for comparison post-injury. Pre-season baseline scores are a tool that may be used potentially following an on field injury. From the base- line scores and the subsequent post-injury score one can determine a change in the patient’s functional status.
Given the deficits that research has found following a concussion, such as reduced reaction time, poor coordination, etc., it is imperative all aspects that could be impacted by a concussion are covered in the assessment and subsequent treatment/management. Therefore, baseline evaluations of athletes to ensure safe return to sport are recommended. A baseline of just one area of the brain, such as only cognitive testing is not enough to ensure that not only are athletes’ brains recovered and not vulnerable to a second concussion, but also that their physical recov- ery is at optimal levels to avoid a potential injury. Symptoms alone are a poor indicator of recovery and therefore baseline objective measures such as orientation, concentration, reaction time, memory, muscular strength, balance, visual processing, cognitive ability, and physical ca- pacity are required to ensure pre-concussion levels are met. Having com- prehensive baseline testing will benefit parents, doctors and therapists by defining the optimal outcomes of individual concussion management.
Going forward…
Far too often concussions go undiagnosed putting the individual at risk of further injury. Once diagnosed a structured, comprehensive approach to rehabilitation and restoring all aspects of a patient’s function, physical, cognitive, and even mental health is imperative. The process involves the collaboration of a number of health professionals including family physi- cians, physical therapists, optometrists, even mental health professionals to help address stress, depression and anxiety which can arise as a result of a concussion. Although rest is important initially after a concussion injury, don’t just wait to feel better. Evidence indicates a more active and struc- tured approach is better. Seek out health care professionals with special- ized credentials and training in the area of concussion management. If you are involved in competitive sports, strongly consider baseline pre-season. Testing the baseline information can be essential in making safe decisions regarding return to play and return to learn for young athletes. |E|
Paul Osadzuk, B.Sc., P.T., MCPA Owner, Physical Therapist | Bayshore Physical Therapy
Rick Thibodeau, B.Sc. Kin., MPT Registered Physiotherapist | Bayshore Physical Therapy
Carolyn Delkus, BSc. (Ex.Sci.), MPT Registered Physiotherapist | Bayshore Physical Therapy